How New Orleans Orthopedic Specialists Diagnose Joint Pain?
New Orleans orthopedic specialists take a detailed approach to diagnosing joint pain. It all starts with an initial consultation where they review the patient’s medical history, looking for past injuries and family histories related to joint issues. A thorough physical exam follows, assessing strength and motion of the affected joints while checking for any visible deformities. If necessary, diagnostic imaging like X-rays or MRIs is ordered to better understand the situation. In some cases, lab tests are performed too. The focus remains on conservative treatment options such as medication and physical therapy before considering surgical interventions if needed. Patient education plays a key role in recovery here.
1. Understanding Joint Pain in New Orleans
Joint pain is a common issue faced by many residents in New Orleans orthopedic specialists, with various factors contributing to this discomfort. It can arise from injuries, arthritis, or autoimmune conditions, and common types include osteoarthritis, rheumatoid arthritis, and bursitis. Lifestyle choices, such as obesity, lack of exercise, and poor diet, can exacerbate joint pain, making prevention and management crucial. Additionally, the humid climate of New Orleans can influence joint discomfort, as some individuals may find their symptoms worsen with changes in weather. Age is another significant factor; as people grow older, they often experience degenerative changes in their joints, leading to increased pain and mobility issues. Active individuals are particularly vulnerable to sports injuries, which frequently result in acute joint pain. Joint pain can affect any joint in the body, including knees, hips, shoulders, and hands. Early detection of symptoms is vital, as it can lead to more effective management and treatment. Chronic joint pain often impacts mental health, with many experiencing depression and anxiety, which can diminish their overall quality of life. Fortunately, New Orleans boasts a range of orthopedic specialists and clinics equipped to address joint pain, providing tailored treatment options to improve patients’ well-being.
- Joint pain can stem from various causes, including injury, arthritis, and autoimmune conditions.
- Common types of joint pain include osteoarthritis, rheumatoid arthritis, and bursitis.
- Lifestyle factors such as obesity, lack of exercise, and poor diet can contribute to joint pain.
- Environmental factors, such as humidity and temperature, may also affect joint discomfort in some individuals.
- Age is a significant factor, as joint issues tend to increase as people grow older, leading to degenerative changes.
- Chronic joint pain may be associated with mental health issues like depression and anxiety, impacting overall quality of life.
- New Orleans has a variety of specialists and clinics available to address joint pain, offering tailored treatment options.
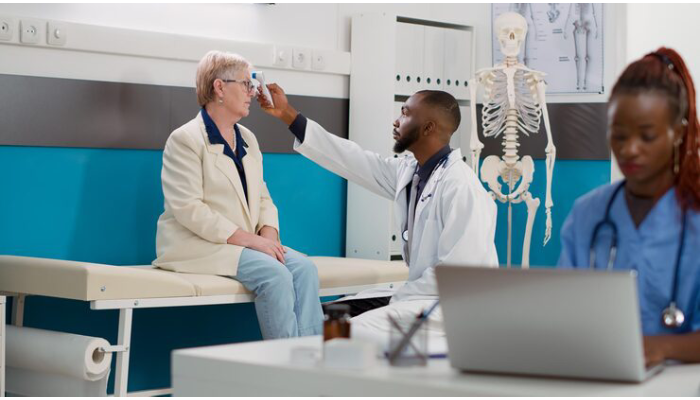
2. Initial Consultation Process with Specialists
During the initial consultation, patients share the details of their joint pain, including how intense it feels and how long they have been experiencing it. Orthopedic specialists often ask about the patient’s physical activity levels and any recent lifestyle changes that may have contributed to their condition. Understanding what the patient hopes to achieve from treatment is also vital, as it helps in tailoring the approach to their needs.
The specialist usually discusses any previous treatments the patient has tried, noting what worked and what did not. Patients are also asked about the medications they are currently on, ensuring there are no potential interactions with new treatments. Specialists encourage patients to bring along medical records or imaging results from past evaluations, as this information can be helpful in forming a complete picture of the patient’s health.
Building a good relationship during this first meeting is important, as it can enhance treatment adherence. Patients learn what to expect in terms of further assessments or treatments, which helps alleviate any anxiety about the process. Additionally, discussing the patient’s support system can provide insights into their recovery journey, making it easier to create a personalized treatment plan that fits their individual needs.
3. Importance of Medical History in Diagnosis
A comprehensive medical history is vital for orthopedic specialists when diagnosing joint pain. By gathering details about past surgeries or injuries, specialists can identify patterns that may contribute to current joint issues. For instance, a history of a ligament tear might explain ongoing knee pain. Additionally, understanding a patient’s family history of joint problems can signal hereditary conditions, such as osteoarthritis, that may affect treatment options.
Moreover, existing medical conditions like diabetes or thyroid disorders can complicate joint health and influence the specialist’s approach. Knowing about allergies and previous reactions to medications is crucial for safe prescribing practices. The timeline of symptoms helps determine whether the condition is acute or chronic, guiding the urgency of treatment.
Lifestyle habits, such as diet and exercise, also play a role in joint health. For example, an inactive lifestyle may worsen joint pain, while a balanced diet can support recovery. Reviewing past imaging or diagnostic tests can provide insights into the progression of joint issues, allowing for more precise treatment plans. Patients should also share any alternative therapies they are using, as this information can lead to a more holistic treatment approach. Accurate documentation of medical history is essential for effective care and follow-up.
4. How Physical Exams Help Diagnose Joint Issues
Physical exams are a key part of diagnosing joint issues. During these exams, specialists assess joint stability, tenderness, and range of motion, which provides critical diagnostic information. They look for signs of inflammation, such as swelling, redness, or warmth around the joint. Functional tests may also be performed to see how well the joint supports movement during daily activities. For instance, if a patient has knee pain, the McMurray test may be used to check for specific issues. The presence of crepitus, a crackling or grinding sound during movement, can indicate underlying joint problems. Additionally, strength tests help identify any muscle weakness surrounding the joint, which may impact its function. Assessing joint alignment is crucial too, as any deformities can affect mobility and pain levels. The physical exam not only aids in pinpointing the issue but also helps rule out other conditions like tendonitis or bursitis that could mimic joint pain. Patient feedback is vital, as it helps the specialist understand pain triggers and limitations. The findings from the physical exam guide decisions on whether further diagnostic testing or imaging is necessary.
5. Role of Diagnostic Imaging in Joint Pain Assessment
Diagnostic imaging plays a crucial role in assessing joint pain by providing a visual representation of joint structures. This aids orthopedic specialists in making accurate diagnoses. Typically, X-rays are the first step, allowing doctors to evaluate bone integrity and identify conditions like fractures or arthritis. For a closer look at soft tissues, MRI scans are invaluable, revealing issues such as ligament tears or cartilage wear. CT scans offer detailed images of bone, which is particularly helpful in complex joint assessments. Additionally, ultrasound can visualize soft tissues and detect fluid accumulation in joints. Results from these imaging tests can confirm or refute initial diagnoses made during the physical exam, guiding specialists in planning effective treatment strategies and predicting outcomes. It’s important for patients to follow specific preparation instructions for imaging tests, like fasting or avoiding certain medications. Over time, imaging findings can also help track the progression of joint conditions, and when combined with clinical assessments, they contribute to a comprehensive approach to patient care.
6. Laboratory Tests for Joint Pain Evaluation
Laboratory tests play a crucial role in evaluating joint pain by providing valuable objective data that supports the findings from patient history and physical examinations. Blood tests can identify inflammatory markers, which help to diagnose conditions such as rheumatoid arthritis. For instance, tests that evaluate antibodies in the blood can rule out autoimmune diseases, giving specialists a clearer picture of the underlying issues. In cases where there is noticeable swelling, joint fluid analysis may be performed to detect infections or conditions like gout.
Additionally, serological tests can reveal diseases impacting joint health, such as Lyme disease. Common tests include a complete blood count (CBC), which assesses overall health and inflammation levels. Markers like C-reactive protein (CRP) and the erythrocyte sedimentation rate (ESR) are particularly useful for gauging the severity of inflammation.
Patients may be required to undergo multiple tests to achieve a comprehensive view of their health status, which can significantly aid in differential diagnosis, ruling out non-joint-related issues. Understanding these lab results is essential for both specialists and patients, as it helps in formulating an effective treatment plan.
7. Evaluating Joint Functionality and Movement
Evaluating joint functionality is a key part of diagnosing joint pain. Orthopedic specialists begin by testing the range of motion in the affected joint to assess flexibility and mobility. This might involve asking patients to move their joints in various directions to see how far they can go without discomfort. Joint stability tests are also performed to check for any abnormal movement that might indicate an injury. For example, if a patient has knee pain, the specialist may perform specific movements to identify what triggers the pain or what limitations exist.
Functional assessments play an important role in determining how joint issues affect daily activities. Specialists may ask patients to perform tasks that mimic their everyday movements, such as squatting, climbing stairs, or walking. This helps to identify any pain or difficulty that could hinder their ability to carry out routine tasks. Additionally, evaluating balance and coordination can provide valuable insights into overall joint and muscle function, revealing any weaknesses that may need addressing.
During this evaluation, specialists often look for signs of joint effusion, which signals swelling or injury. They may also analyze movement patterns to identify compensatory behaviors, where patients unconsciously modify how they move to avoid pain, potentially leading to further problems down the line. All these assessments help in tailoring rehabilitation programs to meet the specific needs of the patient. The findings from these evaluations guide the development of a personalized treatment plan that focuses on improving movement and functionality. Furthermore, understanding joint functionality is crucial for setting realistic recovery goals and expectations, allowing both specialists and patients to work together towards effective pain management and enhanced mobility.
8. Nonsurgical Treatment Options for Joint Pain
Nonsurgical treatments for joint pain focus on relieving discomfort and improving function without invasive procedures. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of defense, helping to reduce pain and inflammation. Physical therapy can play an essential role by strengthening the muscles around the joint and enhancing range of motion, which can lead to long-term improvement.
Weight management is also crucial, as carrying excess weight can increase stress on joints, particularly in the knees and hips. Patients may be advised to adopt lifestyle modifications, such as engaging in low-impact exercises like swimming or cycling, which promote joint health without causing further damage.
Injections, such as corticosteroids or hyaluronic acid, may offer temporary relief from inflammation and pain, serving as a bridge until more permanent solutions can be explored. Assistive devices, including braces or orthotics, can provide support during activities, making it easier to move without pain.
Alternative therapies, like acupuncture or massage, may complement traditional treatments and help alleviate discomfort. Educating patients on joint protection techniques can empower them to manage their conditions better, minimizing stress on affected joints. Heat and cold therapies can also be beneficial, providing relief from pain and stiffness.
9. When to Consider Surgical Interventions
Surgical options become a consideration when nonsurgical treatments do not provide relief after a reasonable period. For individuals suffering from severe arthritis, joint replacement may be recommended if pain severely impacts their quality of life. Additionally, arthroscopic surgery can be performed to repair damaged tissues or remove loose fragments within the joint, helping to restore function. Candidates for surgery are assessed based on various factors, including age, activity level, and overall health status. In cases of acute injuries requiring immediate intervention, surgery may also be necessary to quickly restore functionality. Patients should be well-informed about the risks and benefits associated with surgical options to make educated decisions. Pre-operative evaluations are essential in determining the best tailored surgical approach for each patient’s specific needs. After surgery, post-surgical rehabilitation is critical for recovery, focusing on restoring joint functionality. A multidisciplinary team approach often enhances both surgical outcomes and recovery times, ensuring that patients receive comprehensive care. Informed consent remains a vital part of the process, ensuring patients fully understand the procedure and expected outcomes.
10. Rehabilitation Services After Joint Pain Diagnosis
Rehabilitation services are essential for patients recovering from joint pain or surgery. These programs are carefully designed to restore joint function, strength, and flexibility. Physical therapy sessions focus on exercises that are tailored to the specific joint issues each patient faces. For instance, if someone has a knee injury, their therapy may include targeted exercises to strengthen the surrounding muscles and improve mobility.
In addition to physical therapy, occupational therapy plays a crucial role in helping patients adapt their daily activities. This can involve strategies to manage pain while enhancing overall function. Patient education is also key, as it empowers individuals with self-management strategies to handle their condition effectively.
During rehabilitation, progress tracking is vital. Therapists regularly assess improvements and adjust treatment plans accordingly. They might use modalities like ultrasound or electrical stimulation to aid recovery, providing additional support where needed. Group therapy sessions can also be beneficial, offering motivation and a sense of community among patients facing similar challenges.
11. Patient Education and Follow-up Care
Educating patients about their specific joint conditions is essential for effective management. Orthopedic specialists take the time to explain potential causes of pain and provide symptom management techniques. They discuss the prescribed treatment plan in detail, ensuring patients understand medication dosages and schedules. Patients are encouraged to ask questions about their condition and treatment options, which enhances understanding and compliance with the plan. To support recovery, specialists often provide written materials or resources about joint health, exercises, and necessary lifestyle changes.
Maintaining a healthy weight is emphasized, as it can significantly reduce stress on joints, thereby alleviating pain. Orthopedic specialists explain the role of physical therapy in recovery, outlining what to expect during sessions and recommending at-home exercises to strengthen the affected area. Setting clear expectations for recovery timelines and potential outcomes based on individual conditions allows patients to feel more informed and in control.
Regular follow-up appointments are scheduled to monitor progress, make necessary adjustments to treatment, and address any new concerns that may arise. Patients are also urged to report any changes in symptoms, such as increased pain or swelling, to ensure timely interventions. Engaging in supportive communities or groups focused on joint health is encouraged, as they can provide emotional and practical support during the recovery journey.
Frequently Asked Questions
What tests do orthopedic specialists use to find the cause of my joint pain?
Orthopedic specialists often use several tests like X-rays, MRIs, and blood tests to find out what’s causing your joint pain. These help them see inside your body and better understand the problem.
How do specialists decide whether I need surgery for my joint pain?
Specialists usually look at how severe your pain is, how much it affects your daily life, and what other treatments you have tried before deciding if surgery is necessary.
What should I expect during my first appointment for joint pain?
During your first visit, the orthopedic specialist will ask about your pain, review your medical history, and might perform a physical exam. They may also discuss what tests they plan to do.
Can I do anything at home to help with my joint pain before seeing a specialist?
Yes, you can try resting the joint, applying ice or heat, and taking over-the-counter pain relief medications. However, it is important to see a specialist for proper diagnosis and treatment.
Why is it important to get an accurate diagnosis for joint pain?
Getting an accurate diagnosis is crucial because it helps the specialist determine the best treatment options for your specific condition, leading to better outcomes and improved quality of life.
TL;DR New Orleans orthopedic specialists use a systematic approach to diagnose joint pain, starting with a thorough review of the patient’s medical history and a physical examination. Diagnostic imaging, such as X-rays and MRIs, may be used to confirm findings, while lab tests help rule out specific conditions. Treatment options focus on conservative methods like medication and physical therapy, with surgery considered if necessary. Rehabilitation services and ongoing patient education support recovery and long-term joint health.